Author: Nehal Farouk Twig, Editors: Estelle Mbadiwe and Kenneth Egwu Fri. 31st March 2023. 12:15 PM GMT +1

Background: There is no longer a debate about whether or how quality should be introduced into the healthcare sector because it has become increasingly crucial for businesses to improve their quality and hence increase their competitiveness in today’s globally competitive market (1) There are various ways to look at healthcare quality. From the standpoint of the provider; offering the patient with the highest quality care conceivable. Furthermore, providing cost-effective rationed health care, particularly when resources are scarce, is quality from the administrator’s point of view. On the other hand, from the patient’s standpoint, quality means receiving treatment when and where he needs it, in a timely and safe manner, in line with the goals to cure to cure his disease or ailment (2)
Healthcare, at the global level, has never faced a crisis like the multifaceted experience seen with Covid-19. The effects of the Covid-19 pandemic sparked a paradigm shift that has put the traditional design and operation of health systems under pressure. Governments in Africa and around the world are pouring significant resources into healthcare to address the global healthcare expected emergencies. Even though some healthcare practices that were used during the pandemic, such as social distancing have returned to normalcy, healthcare will still be a hot topic in 2023. Many trends are likely to rule the healthcare and life sciences sector in Africa such as increased Public-Private Partnerships (PPPs) to optimize care access, localization of Pharmaceutical Manufacturing in Africa, telemedicine foundations will be laid out for a wider use across the continent, detailing support and training to Healthcare Professionals will be a mix of face-to-face and remote, pharma will refine Patient Support Programs for a post-COVID-19 world, and demand for mental healthcare will significantly increase (3)
For economic growth and national survival, the quality of the healthcare system as represented in national health indicators becomes crucial. To remain silent over the standard of medical care is to encourage the annual premature death of millions of individuals (4)
State of health systems and service provision in the African Region
The United Nations released updated population forecasts for the world in 2022. The number of people in the WHO African Region is projected to expand by just 0.4% to 2.09 billion by 2050, nearly double the population of Europe and North America. When compared to the global population growth of 1.1% for the year 2020, Africa’s yearly population growth of 2.7% (ranging from 0.8% in Lesotho to 3.7% in Niger) is the greatest in the world. This expansion is associated with a fertility rate higher than anywhere else. In comparison to other regions of the world, the population density in the Region (36 persons per km) is low. In fact, many countries are uninhabitable, yet some countries with a smaller land area have a large population or population concentrations in specific cities. Because of access to various services, population density is particularly an essential metric for the execution of health policy and for governments more widely (5)
According to the quality of care index, just 62.3% of what is feasible is represented by quality of care in the African region. This index ranged from 39.7% to 84.7%, which is a large difference between nations. Above 80% of quality of care index are Namibia, Mauritius, and the Seychelles. Three vital signs are used to gauge the quality of care (monitoring user experience, patient safety, effectiveness of intervention). The user experience of monitoring the vital signs receiving the lowest regional rating (54.9) compared to patient safety (61.0) and the efficacy of the therapies given (70.8). To have the biggest impact on care quality, the Region has to invest comparatively more in interventions like person-centered care initiatives that will enhance overall patient experience during the care process (5)
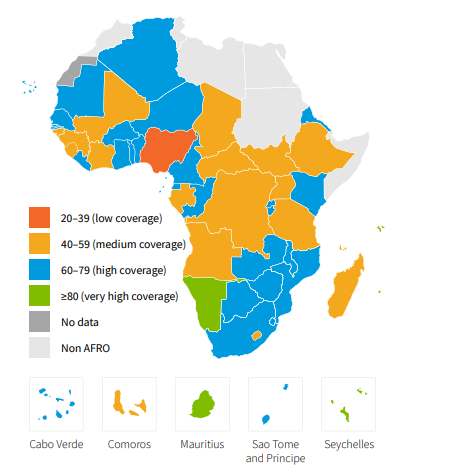
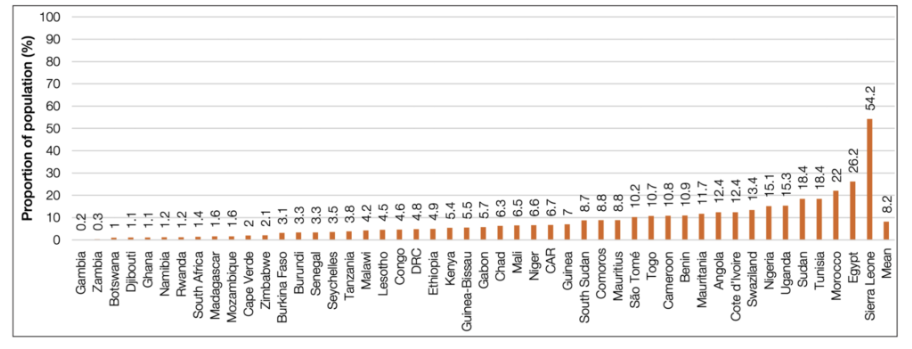
Fewer than half of Africa’s residents (52%) – 615 million people – have access to the healthcare they require, and half of the continent’s women and girls have unmet family planning needs. This is according to a report issued on March, 2021 at the Africa Health Agenda International Conference on Africa’s progress towards achieving universal health coverage (UHC). Every year, roughly 97 million Africans, or 8.2% of the continent’s population, face “catastrophic healthcare costs,” with the highest rates in Sierra Leone, Egypt, and Morocco. According to the research, which was developed by a multi-national Africa Health Agenda International Conference (AHAIC) commission, these out-of-pocket costs will push 15 million people into poverty each year (6)
Despite the fact that Africa’s health outcomes are still fast improving as Health system resilience; resilience describes a systemic approach that links emergency and development; presented a 51.9% score in 2020. The continent still lags behind world regions; far behind in a number of key resilience metrics such as the inbuilt capacity to anticipate, absorb, and transform functionality due to a shock event; and the epidemic preparedness and response core capacity that captures the complementary capacity to respond to a shock event (5) The continent of Africa, in particular, accounts for about 25% of the global disease burden but only 3% of the global health workforce, with just 2.3 doctors and 10 nurses or midwives per 10,000 inhabitants (7)
The WHO Director General’s -report on human resources for health to the World Health Assembly in 2022 revealed there were 3.4 million doctors and 7.4 million nurses in Europe. In comparison, the African region had approximately 300,000 doctors and 1.2 million nurses, Chronic staff shortfalls stifle Africa’s health systems: WHO study found finds that the region has a ratio of 1.55 health workers (physicians, nurses and midwives) per 1000 people. According to WHO threshold density 4.45 health workers per 1000 people needed to deliver essential health services and achieve universal health coverage (8)

Covid-19 Risks and Opportunities on the African healthcare services
The COVID-19 outbreak revealed the gaps in Africa’s healthcare systems. The continent is currently falling behind in COVID-19 vaccination rates. Only 45.6% of Africans have received their full dose of the vaccine. It contrasts with the UK and the US, where, respectively, 75.4% and 69.2% of the population have had all of their vaccinations (9) This gap may have occurred as a result of a number of factors, including the fact that African nations did not place preorders for the alleged vaccines from the manufacturers during the early stages of their development. As a result, the region was forced to rely on the COVAX global vaccine sharing programme of the WHO, bilateral donations, and a late procurement drive from the African Union (AU), which included UNICEF’s commitment to provide 220 million single-dose vaccines by 2022. African countries may be reluctant to administer vaccines because of widespread misconceptions and scepticism over the entire outbreak. The general public may have been affected by the abundance of contradicting COVID-19 information. A lot of Africa’s low-income nations lack the necessary infrastructure and logistics to manage the COVID-19 vaccination campaign. The availability of vaccines, vaccine consumables, and other supplies may be limited (10) On the other side the delivery and administration of healthcare for COVID-19 and other patients benefited greatly from the use of digital solutions in Africa as well as the whole world. First, telemedicine was creatively embraced for clinical treatment in a number of nations (Ex: Eswatini, Rwanda, Ghana, Uganda, and Egypt). Patients were asked to record a video of them taking their prescribed prescription and submit it. Second, during the epidemic, patient and medical staff support was provided by mobile apps and platforms (11)

With almost 65% of the population being under 25, Africa is currently the world’s top example of the demographic shift (changes in the size and structure of the population, caused by changes in birth and death rates), and by 2030, it will account for 42% of all youngsters worldwide. The development and execution of healthcare initiatives at all levels depend heavily on the needs, perspectives, and inventiveness of this cohort. Young professionals bring fresh viewpoints and solutions when given the opportunity to delve deeply into the current healthcare systems. Without enough healthcare professionals, sustainable health systems are impossible. They are the essential element in guaranteeing proper service delivery and coverage. Africa is the fastest-growing continent on earth, but it also has a chronic lack of medical professionals, which the World Health Organization predicts would expand number of workers to 6.1 million by 2030 (9)
Fourth Industrial Revolution innovations and new technology in African healthcare
There exists a positive relationship between improved health care and economic performance, including the importance of the Fourth Industrial Revolution in transforming healthcare, human resources, and economic growth. Experts predict that increased spending on health care in Africa (an average of $21 to $36 per capita annually till the end of 2026) might save 3.1 million lives and result in economic gains of more than $100 billion during that time. Longer life expectancy, greater academic achievement, more savings and investment, lower debt and health care costs, and higher productivity all result from improved health. In fact, the World Health Organization (WHO) predicts that yearly economic growth will increase by 0.4 percent for every 10% increase in life expectancy at birth.
Health and healthcare are becoming more digitalized, and science and medicine are evolving quickly. Given the lack of healthcare workers, infrastructure, facilities, spending, investment, and enabling legislation, among other factors, in the African context, the distribution, transfer, acceptance, adaptation, and, when possible, creation of technology are being used to their advantage by a large number of African entrepreneurs and innovators, notably energetic youth, to meet their immediate health care concerns. African entrepreneurs now have the chance to advance in tackling some of the continent’s ongoing, serious health care concerns, frequently in collaboration with their global counterparts (12)
Conclusion
Investment
in healthcare quality management is essential for Africa’s growth in addition
to improving human lives. The quality of the healthcare system as reflected by
national health indicators becomes essential for both economic growth and
national survival. The quality of care
index in the African region varied significantly. In general, progress has been
observed in almost all areas. The Covid-19 pandemic has caused a paradigm shift
in healthcare planning and management, leading to governments investing in
healthcare to address the crisis.
COVID-19 pandemic, have shown us that although the Region was not
prepared for this particular disease, the response was appropriate and the
pandemic was contained with the fewest possible death. However, statistics also
revealed a disruption in the continuity of health service delivery. Despite considerable advances in terms of
life expectancy and improved access to health care in the WHO African Region,
many challenges remain, such as expected increase in population more than
universal rates, the fact that fewer than half of Africans have access to
healthcare, catastrophic healthcare costs, medical staff severe shortages.
Innovative
technologies which is “marked by the convergence of the digital,
biological, and physical worlds, may have a positive impact on healthcare
provision. Innovations in healthcare promise to have a significant, life-saving
impact on society in addition to opening up new opportunities for the growth of
the healthcare sector. The distribution,
transfer, adaptation, and, creation of technology are being used to their
advantage by a large number of African entrepreneurs and innovators, notably
energetic youth, to meet the healthcare concerns. African countries are at
different stages of achievement of target indicators. The improvement of health
information systems has had an impact on the monitoring of health indicators,
although some key data are still not available. Universal health coverage is
one of these objectives that must be prioritized and to which financial,
infrastructural and human resources must be allocated. The use of data for
decision making will create a strong paradigm shift for appropriate strategic
planning and implementation.


Africa health systems are clear reflection of healthcare inequity.
Great work Dr. Nehal, wishing you all the best